We discussed a case about a middle-aged woman with history of cluster migraines, presenting with chronic headaches & acute left eye optic neuritis and left CN V1-3 palsy, found to have neurologic sarcoidosis.
Sarcoidosis is a granulomatous disease that can affect all organ systems. It causes non-necrotizing (non-caseating) granulomas.
Epidemiology
- African Americans 2-3x > Caucasians
- Females 2x > males
- Young adults
Pulmonary sarcoidosis
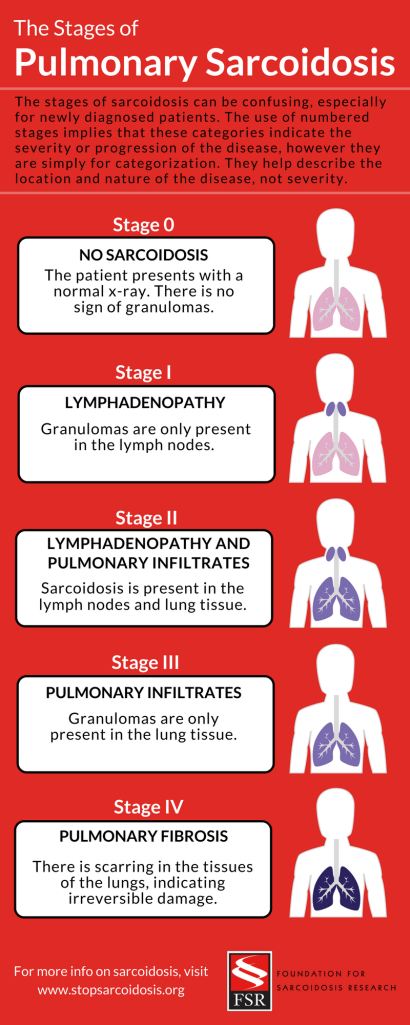
Chest radiographic findings are organized into stages. This gives an anatomic guide to lung involvement, but does not reflect disease activity or functional deficits.
- Stage I:
- Bilateral hilar adenopathy
- Stage II:
- Bilateral hilar adenopathy and parenchymal involvement (most commonly reticulonodular opacities)
- Stage III:
- Parenchymal involvement without adenopathy
- Stage IV:
- Fibrosis
Extrapulmonary sarcoidosis
- Sarcoidosis can affect all organs
- Most common extrapulmonary involvment
- Skin
- Eyes
- RES
- MSK
- Exocrine glands
- Heart
- Kidney
- CNS
Ocular Sarcoidosis
- Affects up to 25% of pts with sarcoidosis
- Females > males
- More common in African American and Japanese populations
- Intraocular: uveitis
- Extraocular: lacrimal glands, conjunctiva, extraocular muscles, optic sheath
Lofgren syndrome
A specific acute presentation of sarcoidosis.
Classic triad of:
- Bilateral hilar lymphadenopathy
- Erythema nodosum
- Arthropathy
Treatment
- Initial: glucocorticoids
- Refractory / intolerant to steroids: immunosuppression agents (MTX, azathioprine, leflunomide, or TNFα inhibitors