Cauda Equina Syndrome:
Cauda Equina: set of intradural nerves that provide sensory/motor innervation from L2-S5
Nerve Roots of Cauda Equina:
- Hip muscles
- Lower extremity muscles
- Urinary and anal sphincters
- Sexual organ muscles
Causes of Cauda Equina:
- Disc herniation (MOST COMMON)
- Lumbar stenosis (OA)
- Trauma
- Infection/abscess
- Metastatsis/neoplasma (Metastasis most common, ependymoma or schwannoma possible)
- Inflammatory disease (CIPD, Paget’s, ankylosing spondylitis)
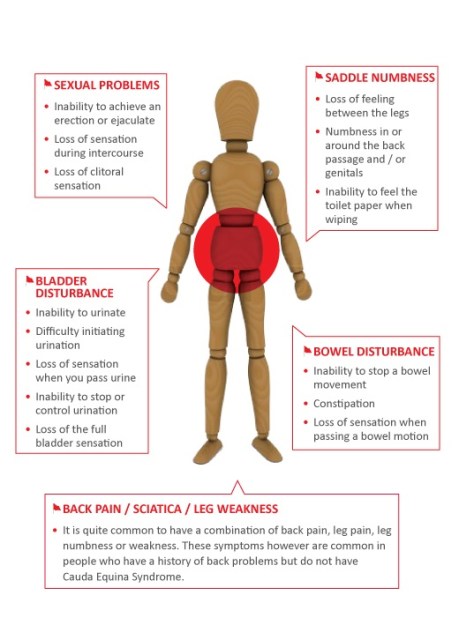
Symptoms – based on level
Low back/radiating LE pain with at least one below
- Urinary incontinence/retention
- Fecal incontinence/retention
- Loss of anal sphincter tone
- Sexual dysfunction
- Saddle anesthesia/hypoesthesia
Treatment:
– urgent neurosurgical evaluation to reduce side/eliminate mass
– eradicate causative organisms
Most common organisms:
– staph (63%)
– strep (9%)
– gram negative anaerobes (16%)
Empiric antibiotic regimen: vancomycin and cephalosporin +/- nafcillin
Steroids indications:
– within 8 hours of traumatic spinal cord injury
– metastatic disease (followed by surgery/radiation)