Remember the different dimorphic fungi:
- Histoplasma capsulatum
- Blastomyces dermatitidis
- Coccidioides immitis
- Paracoccidiodies brasiliensis
- Sporothrix schenckii
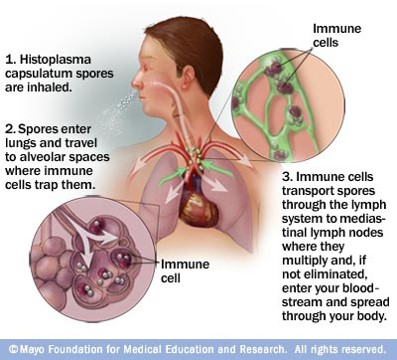
Histoplasma infection route: spores are inhaled (remember the association with bats and caves), enter the lungs and travel to the alveolar spaces where immune cells trap them. The spores are then spread through the lymph system to mediastinum where they can enter your blood stream.
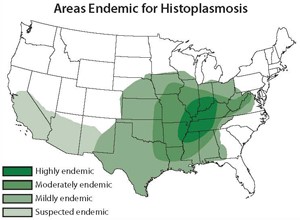
Think of histoplama when a patient presents with symptoms after traveling to an endemic area:
Disseminated histoplasma can affect various systems:
GI: approximately 70% have GI involvement at autopsy, but manifestations occur in <10% of patients. Can cause HSM, but typically results in ulcers/polypoid masses in the colon and ilium.
Skin: reported in 10-15% of disseminated histoplasma; more common in patients with AIDs. Lesions typically include nodules, papules, plaques, ulcers, vesicles, and generalized dermatitis.
Adrenal: common (80-90%) of autopsy cases, but overt adrenal insufficiency is rare – <10% of cases.
CNS: occurs in 5-20% of patients with disseminated histoplasma; more common in immunosuppressed individuals.
*Be able to recognize blastomyces (broad based budding yeast) and cocciodioidomycosis (thick walled spherules with endospores) on histology.
Treatment:
Amphotericin B (lipid formulation): recommended for patients sufficiently ill to require hospitalization; itraconaozle not recommended because it does not eradicate fungemia as rapidly.
Itraconazole: treatment of choice for mild/moderate symptoms and as step-down for people improving on amphoterician B.
