Wernicke’s Encephalitis (WE) Triad:
1) Encephalopathy
2) Ataxia
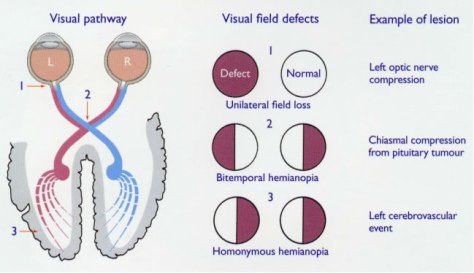
3) Oculomotor dysfunction
* presence of all 3 symptoms is not needed in order to make the clinical diagnosis; only approximately 10% of patients will display all 3 symptoms.
Korsakoff Syndrome (additional 2 findings):
4) Selective anterograde/retrograde amnesia
5) Confabulation
WE is an under-recognized disease with a prevalence of 0.4 – 2.8% in the general population and up to 12.5% in alcohol abusers.
WE is more common in men, but women are more susceptible to development.
Caine Criteria – proposed in 1997 (article below) – only need 2 of 4 for diagnosis
1) Dietary deficiency
2) Oculomotor dysfunction
3) Cerebellar dysfunction
4) AMS or mild memory impairment
* study of 106 autopsied alcoholics found that use of the Caine criteria from the standard WE triad increased the diagnostic sensitivity from 22% (classic triad) to 85% (Caine criteria).
Remember that WE can be associated with a number of conditions/diseases (not a compelte list):
– Chronic alcoholism
– Anorexia/dieting
– GI surgery (esp. bariatric)
– Dialysis
– Prolonged IV feeds without supplementation
– Sepsis (high catabolic state)
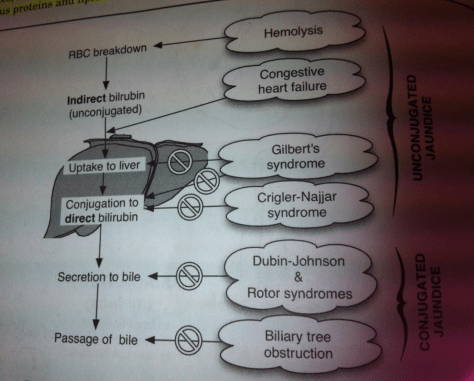
Pathophysiology – WE is due to thiamine (vitamin B1) deficiency. Remember to WE is a clinical diagnosis and treatment should be started early to prevent irreversible damage. Response to therapy may be diagnostic.
No lab testing is needed for diagnosis!
Treatment:
Thiamine IV 500 mg TID Days 1-2
Thiamine IV 250 mg BID Days 3-5
Thiamine PO 100 mg daily, which should be continued until the patient is no longer at risk.
* Avoid glucose before thiamine if possible – can precipitate an episode of WE.