- 5 Classic Causes of Hypoxemia
- V-Q Mismatch (elevated A-a gradient)
- Diffusion problems (elevated A-a gradient)
- Shunting (right to left shunt, PE) (Elevated A-a gradient)
- Hypoventilation (normal A-a gradient)
- Altitude, low inspired FiO2 (normal A-a gradient)
- Illness script for PCP Pneumonia: Usually HIV +, chronic non-productive cough (due to high viscosity of sputum), often normal lung exam and chest film, may see ground glass opacities in the bilateral lower lung fields, hypoxia worse with exertion
- Start steroids in addition to Bactrim for FiO2 < 70 or A-a gradient > 35, treatment of PCP fungal death causes a profound inflammatory reaction which is why steroids decrease mortality, treatment course is for 21 days
- Prophylaxis for PCP in HIV for CD4 < 200, 95% effective in preventing PCP
Category Archives: Morning Report
Resident Report 2/1 – Periodic Paralysis
Teaching Pearls:
- Periodic Paralysis occurs as a result of genetic channelopathies that can cause bilateral UE and LE weakness
- More pronounced in proximal vs distal muscle groups
- No loss of bulbar muscle functions or respiratory muscles
- Hypo or a-reflexic on exam
- Evidence of hypokalemia on labs.
- Seen in younger patients <20 years of age.
- Symptoms occur during rest after strenuous exercise, high carbohydrate diet, fasting state
- Primary acquired cause of periodic paralysis is due to thyrotoxicosis
- Theorized to increased Na/K channels causing hyperpolarization, making it harder to reach threshold to set off action potential.
- Classically seen in Asian young males
- Seen in younger patients >20 years of age.
- Differential Diagnosis
- Myasthenia Gravis
- Bulbar muscle involvement that gets worse with activity
- GBS
- Ascending motor and sensory involvement, symmetric
- Tick Paralysis
- Motor abnormalities, no sensory defect, asymmetric
- Botulism
- Bulbar involvement, spread in craniocaudal direction
- Acute myelopathy
- Motor involvement, hyperreflexic
- Myasthenia Gravis
- Treatment
- Treat underlying etiology of periodic paralysis
- Behavioral modification
- Avoid strenuous exercise and high carbohydrate meal intake
- Oral medications
- Consider acetazolamide
- Consider spironolactone
Resident Report 1/28 – Hemolysis
A special thank you to Dr. Lee Levitt for coming to morning report to participate in this interesting case!
Teaching Pearls:
- Discrepancy of a low O2sat along with normal PaO2 is classically seen with methemoglobinemia.
- Other causes include poor perfusion state such as vasoconstriction, hypothermia, or any other conditions that cause poor flow state.
- Methemoglobin – Iron within hemoglobin exists as the oxidized state (+3), causing decreased affinity for oxygen binding.
- Carboxyhemoglobin – when carbon monoxide binds to hemoglobin.
- Hemoglobin has a very high affinity for CO compared to O2. Causes the oxygen dissociation curve to shift to the left, leading to decreased ability for O2 unloading.
- Pulse oximetry cannot distinguish between carboxyhemoglobin and oxyhemoglobin.
- Workup of anemia
- Underproduction
- Blood loss
- Increased destruction (hemolysis)
- Reticulocyte count – important to correct for degree of anemia and time of maturation.
- High corrected reticulocyte index suggestive of blood loss or hemolysis.
- Low corrected reticulocyte index suggestive of underproduction.
- Hemolysis Labs
- High LDH, low haptoglobin, indirect hyperbilirubinemia, Coombs test
- Blood Smear
- Schistocytes, helmet cells suggestive if microangiopathic hemolytic anemia.
- Bite cells and Heinz bodies suggestive of G6PD deficiency.
- Spherocytosis suggestive of either hereditary spherocytosis or autoimmune hemolytic anemia.
- Sickle cells suggestive of sickle cell anemia
- Target cells suggestive of liver disease (in particular obstructive liver disease), hemoglobinopathy, etc
- Causes of Intrinsic hemolysis
- RBC membrane defects
- Example includes hereditary spherocytosis
- Hemoglobinopathy
- Examples include thalassemia, sickle cell disease, etc
- Oxidation Problem
- Most common example is G6PD deficiency.
- RBC membrane defects
- G6PD Deficiency
- Different variants of disease spectrum
- X-linked disease – manifest in males
- Hemolysis precipitated by acute insult, including infections or medications.
- Medications associated with hemolysis include primaquine, dapsone, sulfa medications, etc.
- Mediterranean variant associated with favism.
- Negative G6PD test does not rule out G6PD deficiency in the setting of hemolysis.
Morning Report 1/27/16
Great Discussion today! Thanks to Mike Cruz for presenting.
- Remember that isopropyl alcohol and ethanol causes an osmolar gap without an anion gap.
- Beware of a normal osmolar gap in a patient with a positive volatile screen – this could reflect complete conversion of the parent compound to toxic metabolites
| Name | Anion Gap | Osmolar Gap | Toxicity | Treatment |
| Methanol | ELEVATED | YES | Retinal Toxicity from Formic Acid | Fomepizole |
| Ethylene Glycol
(antifreeze) |
ELEVATED | YES | Renal Failure, Oxalate crystals | Fomepizole, Ethanol |
| Propylene Glycol
(IV Lorazepam) |
ELEVATED | YES | Lactic Acidosis
CNS depression |
HD if severe |
| Isopropyl Alcohol
(rubbing alcohol) |
NORMAL | YES | Sedation | Supportive Care |
| Ethanol | NORMAL | YES |
Hypocalcemia
- MKSAP Question: Illness script for Asian female with metastatic lung adenocarcinoma – check for the EGFR mutation
- Approach to Hypocalcemia: Check the PTH level. Causes of hypocalcemia with high PTH include Vit D resistance, pancreatitis, CKD. Causes of hypocalcemia with low PTH include destruction of the parathyroid gland (autoimmune, surgery).
- Clinical Manifestations of Hypocalcemia: Peri-oral numbness, paresthesias, tetany, seizures, papilledema, etc
- Tetany = neuromuscular irritability
- Chvostek’s Sign
- Trousseau’s Sign
- Indications for IV Calcium drip
- Rapid drop of total calcium to < 7.5
- Symptomatic hypocalcemia (tetany, carpopedal spasm, seizures)
- Prolonged QTC
- The two main causes for hypocalcemia in ESRD are hyperphosphatemia (inability to excrete phosphorous) and lack of calcitriol production by the kidney.
- Treatments for secondary hyperparathryoidism in ESRD include phosphorous binders, calcitriol, and calcimimetics.
Intern Report 1/27 – Hypercalcemia
Teaching Pearls:
- Primary hyperparathyroidism and malignancy comprise of >90% of cases of hypercalcemia.
- Primary hyperparathyroidism is the most common cause of hypercalcemia in outpatient settings.
- Patients are often asymptomatic and/or have a history of kidney stones
- Malignancy is the most common cause of hypercalcemia in inpatient admissions.
- Labs often display severe hypercalcemia
- Patients with severe hypercalcemia are often volume depleted as hypercalcemia can lead to nephrogenic diabetes insipidus
- Initial Workup – First measure the PTH level
- High PTH: diagnosis is likely primary hyperparathyroidism
- High normal to mild elevation: think of primary hyperparathyroidism or Familial hypocalciuric hypercalcemia (FHH)
- Low PTH: proceed onto further tests
- Other work-up labs include PTHrP and vitamin D metabolites. Other considerations include SPEP/UPEP, TSH, Vitamin A, etc.
- FHH differs from primary hyperparathyroidism in that the fractional excretion of Ca in FHH is low, whereas primary hyperparathyroidism is high.
- Decreased fractional excretion of Calcium leads to lack of nephrolithiasis development.
- Primary hyperparathyroidism has three different pathologic conditions:
- Adenoma – 89-90%
- Hyperplasia – 6.8%
- Carcinoma – 1.2%
- Should consider parathyroid carcinoma in patients with primary hyperparathyroidism and the following:
- Severe elevations in calcium
- Severe elevations in PTH
- Management
- IV fluids NS at 200-300cc/hour to maintain UO at 100-150cc/hour.
- Loop diuretics only used in the setting of fluid overload
- Calcitonin – onset of action: hours
- Concern for tachyphylaxis
- Bisphosphonates (pamidronate or zolendronate)
- Onset of action >2 days
- IV fluids NS at 200-300cc/hour to maintain UO at 100-150cc/hour.
Intern Report 1/19: Sarcoidosis
Teaching Pearls:
- Presents in 20-60 year old individuals. Diagnosis tends to occur 10 years earlier in blacks than Caucasians.
- Over 90% present with pulmonary findings on imaging.
- About 50% of patients with sarcoidosis are asymptomatic.
- About 30% of patients with sarcoidosis have extrapulmonary manifestations
- Extrapulmonary manifestations include:
- Cutaneous – can be found on tattooed skin
- Cardiac – monitor for conduction delays, infiltrative heart diseases
- Lymph nodes, liver, spleen
- GI
- Renal
- Systemic symptoms
- Differential Diagnosis
- Infectious
- HIV, TB, fungal lung diseases
- Occupational/environmental toxin exposure
- Hypersensitivity pneumonitis
- Pneumoconiosis (Beryllium)
- Langerhans Cell histiocytosis
- Malignancy (lymphoma)
- Infectious
- Diagnosis is made with the following:
- Clinical and radiographic findings
- Excluding other potential causes
- Tissue biopsy
- Lofgren’s syndrome
- Erythema nodosum, bilateral hilar adenopathy, fever, arthritis
- Biopsy not needed if Lofgren’s syndrome is present (high specificity)
- Prognosis – fantastic; treatment – NSAIDs
- A Boards favorite topic. (Very high yield)
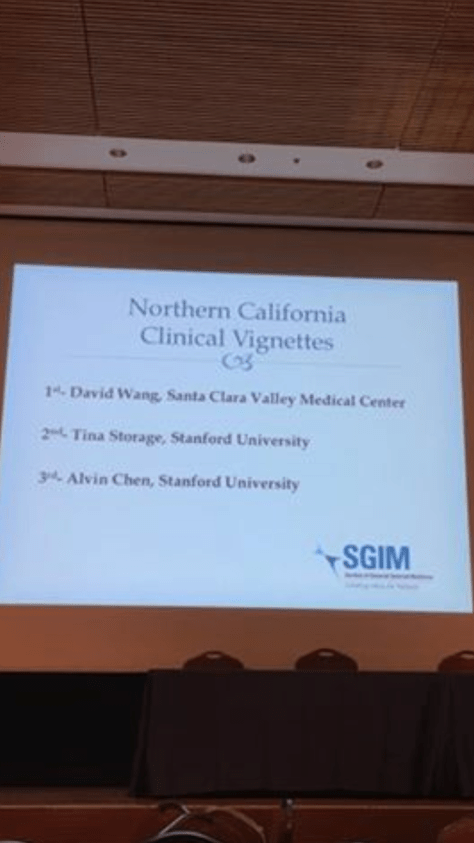
SGIM Poster Presentations
Congratulations to our 8 poster presenters for representing the VMC family at SGIM Northern California-Hawaii Conference!
Our very own David Wang scored FIRST PLACE on his poster presentation!!! Congratulations again!!
Resident Report 1/14 -Thrombosis
Teaching Pearls:
- Inherited Thrombotic Diseases
- Factor V Leiden
- Moderate risk of thrombosis
- Prothrombin G2120A mutation
- Moderate risk of thrombosis
- Protein C Deficiency (higher risk of thrombosis)
- Protein S deficiency (higher risk of thrombosis)
- ATIII Deficiency (higher risk of thrombosis)
- Factor V Leiden
- Factor V Leiden is the most common inherited thrombotic disease
- Occurs in 5% of Caucasians
- Heterozygotes have 5-fold increase in thrombosis; double hit has 50-fold increase.
- Treatments for coagulation reversal
- FFP
- Plasma containing normal factors
- May take 1-2 hours for action
- Higher volume load
- Kcentra
- Concentrate with factors II, VII, IX, and X
- Immediate
- Vitamin K
- Duration of action approximately 4-12 hours
- FFP
Resident Report 1/13 – SJS/TEN
SJS/TEN Teaching Pearls:
- SJS/TEN are severe mucocutaneous lesions
- <10% of epidermal involvement categorized as SJS.
- >30% of epidermal involvement categorized as TEN
- 10-30% of epidermal involvement categorized as SJS/TEN
- Most commonly caused by:
- Medications (allopurinol, anticonvulsants, sulfonamides, NSAIDS)
- Infectious (mycoplasma pneumonia, CMV)
- Clinical Manifestations:
- Prodrome of fever and flu-like symptoms 1-3 days
- Development of mucocutaneous and skin lesions that start as erythematous macules.
- Progress to vesicles and bullae formation within days prior to sloughing.
- Mucocutaneous involvement occurs in >90% of patients (oral, ocular, urogenital).
- Complications
- Fluid balance and electrolyte abnormalities
- Infections
- Staph Aureus and Pseudomonas
- Fungemia
- No role for empiric antibiotics.
- Pulmonary
- ARDS
- Pneumonia
- Management
- High level of suspicion as early withdrawal of medications important for treatment.
- Symptomatic care
- Consult ophtho, burn, and derm
- Patient should be transferred to ICU burn care if moderate to high severity of disease.
| Dinstiguishing Features | DRESS | SJS/TEN |
| Rash Morphology |
Erythroderma, swelling, maculopapular rash
|
Vesicle/bullae formation followed by sloughing |
| Localization |
Diffuse, usually involves the face.
|
Diffuse; often spares the palms/soles, and scalp |
| Timing |
Occurs 2-8 weeks after medication intake
|
Occurs 3-21 days after medication intake |
| Internal Organ Involvement |
Lymphadenopathy, renal (AIN), hepatitis
|
Due to result of complication from SJS/TEN |
| Systemic signs | Fever, malaise, fatigue
|
Fever, malaise, odynophagia |
| Lab Findings |
Eosinophilia
|
Lymphopenia, rarely eosinophilia |
