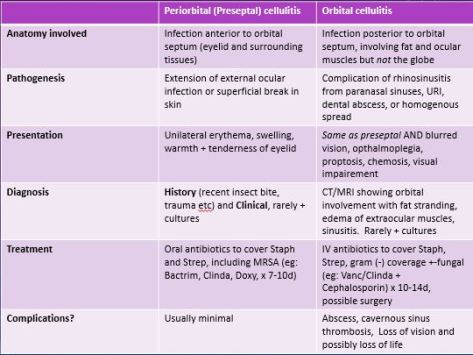
Distinguishing Pre-septal cellulitis (peri-orbital) and Orbital cellulitis
Acute angle closure glaucoma
Clinical presentation
–Elevated IOP presenting as vision loss, acute SEVERE eye PAIN, frontal headache, nausea/vomiting with exam commonly showing corneal edema or cloudiness and mid-dilated pupil reacting poorly to light
This is an eye emergency!
Treatment
You either want to DECREASE aqueous humor production or INCREASE OUTFLOW by constricting the eye. NEVER dilate the eye as it can decrease outflow and increase IOP
-Beta blockers, Acetazolamide, Mannitol (decrease production of aqueous humor)
-Alpha agonists, Pilocarpine (increase outflow)
Hypermucoid variant of KIebsiella Pneumoniae
–Hypermucoviscosity virulence factor
-Diagnosed in lab via STRING test and positive result is >5 mm viscous string from colony on agar plate
-Important to distinguish from non-virulent form as associated with metastatic involvement (endophthalmitis, meningitis, brain abscess but can go anywhere in the body). -Always check with the lab if not reported!

KLA (Klebsiella Liver Abscess)-associated with Hypermucoid Klebsiella
-PRIMARY liver abscess in absence of hepatobiliary disease, diagnosed via ultrasound or CT scan
–Risk factors include DMII, prior antibiotic use, and being of Asian descent (commonly from Taiwan)
-Commonly presents with Fever (93 %), RUQ pain, N/V, leukocytosis, elevated alkaline phosphatase (78 %) and elevated AST/ALT (68 %)
Treatment of Hypermucoid Klebsiella
-Empiric treatment with Cephalosporin (commonly CTX) and Flagyl for empiric therapy, adjust based on sensitivities
–Drainage of liver abscess if present (will not improve with antibiotics alone!)