Before considering HOCM, think about secondary causes of hypertrophic cardiomyopathy
-HTN
-Aortic Stenosis
Disease manifestations of Hypertrophic Cardiomyopathy
-LV outflow tract obstruction due to thickened septum (see picture below)
-Diastolic dysfunction
-Myocardial ischemia
-Mitral regurgitation

Clinical symptoms of HOCM
–Heart Failure (90 % present with DOE), due to LVOT, diastolic dysfunction, and MR
–Chest pain
–Arrhythmias-SVT and VT-risk of sudden cardiac death!
–Syncope
How to make the diagnosis?
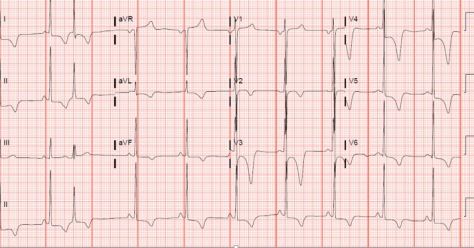
Start with an EKG!
-Look for severe LVH and biatrial enlargement, can suggest HOCM. Due to asymmetrical hypertrophy, can see deep Q waves in the lateral and inferior leads.
What do you see in this EKG of our patient who was found to have a new diagnosis of HOCM? See below for the answer
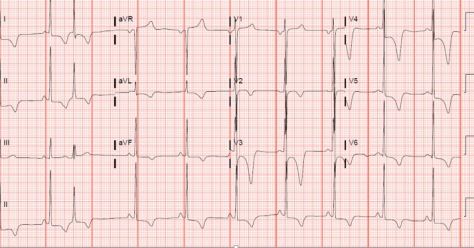
Severe LVH. Biatrial enlargement, deep T wave inversions throughout
–Echocardiogram-see unexplained LV wall thickness >15 m (makes diagnosis), commonly asymmetric septal hypertrophy. Can also see SAM (systolic anterior motion of mitral valve, worsening obstruction), and LVOT.
Further workup
–Ambulatory EKG monitoring: 24-48hr Holter to evaluate for arrhythmias
–Exercise stress test-Risk stratification, GXT preferred. Evaluate degree of LVOT if not seen on echocardiogram
–Cardiac MRI-risk stratification due to better visualization than TTE
-Note that genetic testing is NOT routinely done due to 11 genes, and >1500 mutations responsible, but can be considered as Autosomal Dominant inheritance.
–Cardiac catheterization not routinely done unless high suspicion of ischemia
Medical treatment
-LOWER heart rate and DECREASE inotropy
-3 classes of medications commonly used
–BETA BLOCKERS (first line)
–Nondihydropyridine CCB (commonly Verapamil)
–Disopyramide
-Classes of medications to AVOID
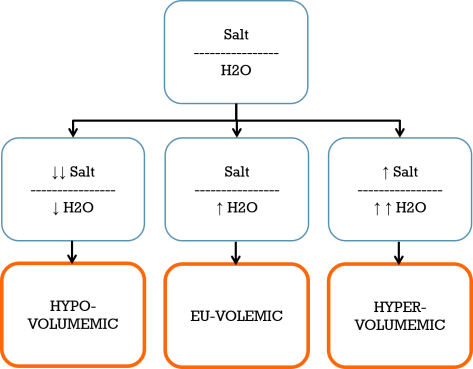
–Diuretics-reduction in preload can worsen LVOT (don’t let them become hypovolemic!)
–Vasodilators– decreased peripheral resistance can increase LVOT obstruction
–Positive Inotropes (eg: Dobutamine)
Non-pharmacologic therapies
1)Activity restriction-avoid high intensity exercise, need to be counseled on this as HOCM is the number one cause of sudden cardiac death in those under age 30!
2)Alcohol septal ablation
3)Surgical myomectomy
Who needs to get an AICD?
Only if you are HIGH risk based on risk stratification
-Highest risk if history of prior sudden cardiac arrest or sustained ventricular arrhythmias
Other high risk features include:
-Family History of SCD
-Syncope
-NSVT
-Massive LVH>30 mm
Not everyone needs an AICD, eg: if asymptomatic and negative family history!







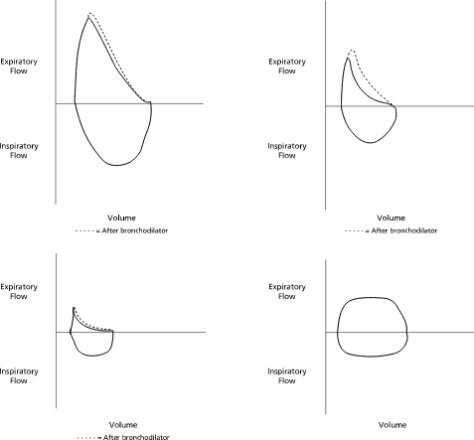 Top Right: Normal; Top Right: Asthma, Bottom Left: COPD, Bottom Right: Fixed Obstruction / Tracheal Stenosis
Top Right: Normal; Top Right: Asthma, Bottom Left: COPD, Bottom Right: Fixed Obstruction / Tracheal Stenosis