- Remember the risk factors for AQUIRED THROMBOPHILIA:
- Surgery (OR 21.7)
- Trauma (OR 12.7)
- Hospital/SNF (OR 8.0)
- Cancer undergoing chemotherapy (OR 6.6)
- Others: estrogen therapy, pregnancy, obesity, smoking
- Approximately 6% of patients with unprovoked VTEs have an undiagnosed cancer at the time of the VTE; approximately 10% will be diagnosed with cancer in the following year.
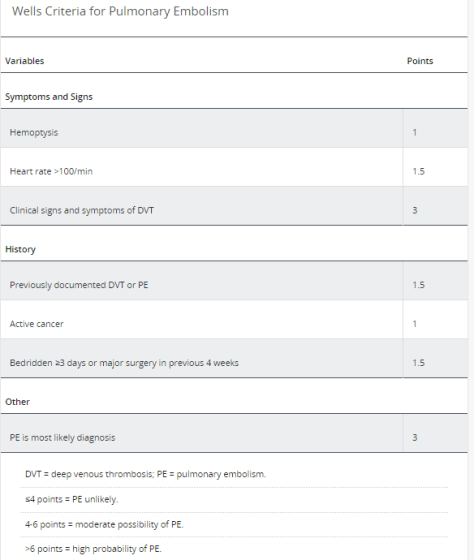
- Use the Well’s PE Criteria for those patients whom you suspect a PE; if the score is <6 consider a D-Dimer to guide management
EKG findings in PE:
- Sinus tachycardia: approximately 44% of patients
- S1Q3T3 (acute cor pulmonale): not sensitive/specific; found in 20% of patients with PE
- RV strain patter (TWI R precordial leads V1-V4): representative of elevated PA pressures; found in approximately 34% of patients
Indications for Thrombolytics in PE:
CLEAR INDICATIONS:
- Persistent hypotension / shock due to an acute PE
POSSIBLE INDICATION:
- Severe / Worsening RV Dysfunction
- Cardiopulmonary arrest due to a PE
- Extensive clot burden
- Free floating RA / ventricular thrombus
- Patient foramen ovale
Contraindications to thrombolytics:
- Intracranial neoplasm
- Intracranial / spinal surgery or trauma
- History of hemorrhagic stroke
- Active bleeding
- Any stroke within 3 months
Classification of PE and distinction:
Massive: cardiopulmonary shock or hypotension
Submassive: RV dysfunction / elevated cardiac biomarkers
Low Risk: normal echocardiogram / negative cardiac biomarkers