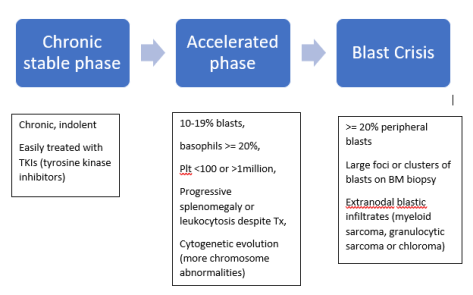
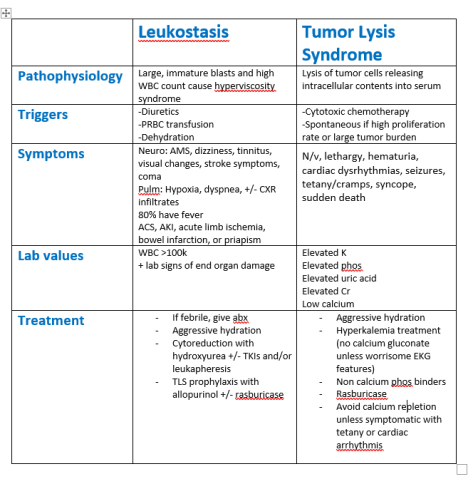
Today’s case was a middle-aged male with a history of untreated CML who presented with gum bleeding, hypoxia, and altered mental status, found to have accelerated phase CML, leukostasis, and tumor lysis syndrome.
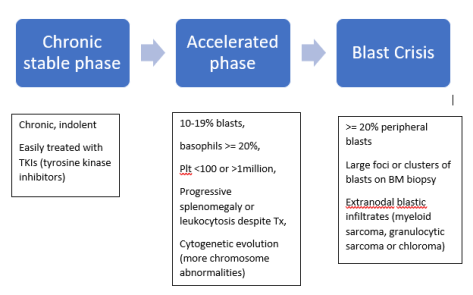
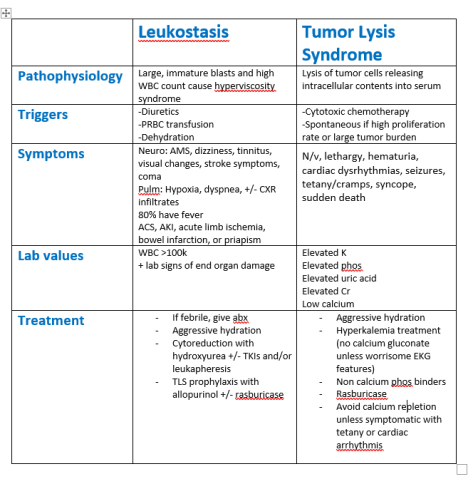
Today’s case was a middle-aged male with a history of untreated CML who presented with gum bleeding, hypoxia, and altered mental status, found to have accelerated phase CML, leukostasis, and tumor lysis syndrome.
Today we discussed an interesting case of acute encephalopathy due to hypercalcemia of malignancy due to bone metastases.
We first reviewed the importance of maintaining a broad differential for acute encephalopathy/delirium/acute confusional state/AMS.
We reviewed the following framework:
Neurologic / Toxic / Metabolic / Infectious / Other.
We then reviewed the differential for hypercalcemia. For those of you interested, please check out this awesome review video by Dr. Strong:
Our patient had hypercalcemia of malignancy and the following patients were made:
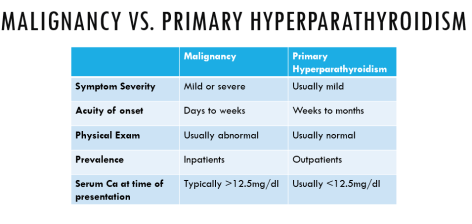
Finally, here is a way to distinguish between malignancy related hypercalcemia and primary hyperparathyroidism (most common cause in outpatients & higher co-occurrence in patients with malignancy)
For treatment options, please see the following blog post for more details!
Today’s case presented by Dr. Neharika Khurana was an elderly male with a history of tobacco use who presented with subacute/chronic cough, unintentional weight loss, night sweats, and hyponatremia.
Our general approach to hyponatremia:

*Diuretics create a high urine sodium regardless of volume status unless severe dehydration is present
*If renal disease or intracranial pathology (cerebral salt wasting syndrome) is present, urine sodium may be high when the volume status is actually low
Today we discussed a case of a gentleman with a recent hospitalization for bacteremia who presented with hypertension, renal failure, nephrotic range proteinuria and dysmorphic RBCs consistent with a glomerulonephritis. We learned the following, pathological-based approach to classifying GNs.

Courtesy: AccessMedicine
Infection-Related GN (IRGN)
Today we discussed a fascinating case of statin-related anti-HMGCR positive immune-mediated inflammatory myositis (also called necrotizing autoimmune myositis). The case highlighted the importance of a framework approach to diseases.
We first went over the framework for true muscle weakness, which can be anatomically divided as follows
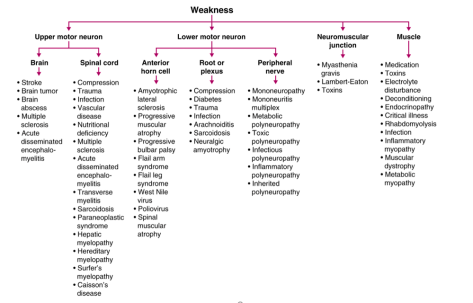
Source: Frameworks for Internal Medicine (Dr. Andre Mansoor from OHSU). Available on Amazon (highly recommended!)
To help us localize the lesion to a myopathy, we used the following framework to determine that it was likely a myopathy.

The differential for myopathy is broad, and generally is the same for an elevated CK and non-traumatic, non-exertional rhabdomyolysis. The causes can be divided as follows. If you like mnemonics, think Drug-REGIIME for the various categories.

Once we narrowed the differential to an inflammatory myopathy, we utilized the following chart that guided us to the probable conclusion that it was an immune-mediated necrotizing myopathy (also known as necrotizing autoimmune myopathy). This was confirmed by a highly positive anti-HMGCR antibody
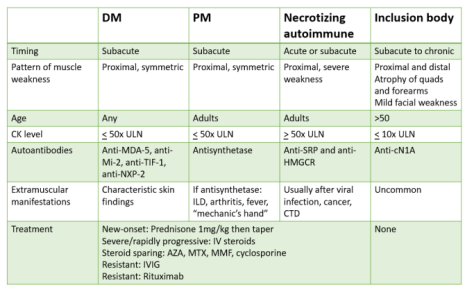
Adapted from a NEJM Article: https://www.nejm.org/doi/full/10.1056/NEJMra1402225
Clinical Pearls about INMN/NAM:
Today’s case was a 60-year-old man with acute onset atypical chest pain, tachycardia, mild leukocytosis, and concave ST elevations without anatomical distribution, who was found to have acute pericarditis.

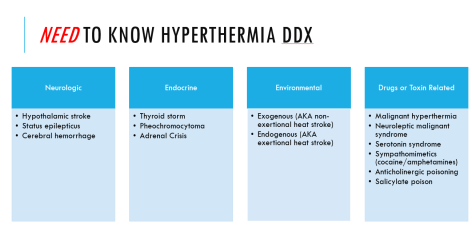
We learned about a patient who presented with a heat stroke during our recent heat wave. Remember the importance difference between fever and hyperthermia
Fever: elevation of hypothalamic set-point leading to increased core temperature
Hyperthermia: elevation of core temperature independent of changes in the body’s thermoregulatory center.
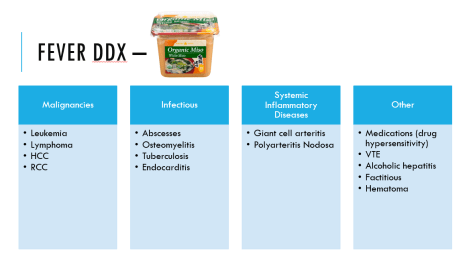
In clinical practice it is often difficult to discern the two – and therefore for challenging cases, it may be useful to think about the differentials for both. Remember, everyone NEEDs MISO 🙂
Thanks to Phuong today for presenting the case of a young woman who presented with volume overload, found to have constrictive pericarditis!
Clinical Pearls

We also talked about a helpful way of breaking up new onset ascites to help generate a DDx:

Today, we talked about the case of a middle aged woman with recent diagnosis of metastatic breast cancer on palliative Paclitaxel who was admitted with acute onset of bloody diarrhea found to have Shiga toxin and progression to HUS! She developed neurologic manifestations for which she underwent PLEX and is now recovering in rehab.
Clinical Pearls
Moral of this story: start PLEX while you’re waiting to decide if it’s HUS or TTP!
Thanks to Paige for presenting the case of a middle aged homeless man who presented with heart failure exacerbation, found to have digital ischemia and subsequently diagnosed with scleroderma and likely contribution from cocaine-induced Raynaud’s!
Clinical Pearls
Large vessel
Medium vessel
Small Vessel
Screen for malignancy in patients with new diagnosis of scleroderma!
Extracutaneous disease:
Management: