







Most common etiologies of AS
Symptoms
Diagnosis
Low-flow, low-gradient AS
When to treat?
Treatment







Mechanism of action:
Clinical features
Diagnostic tests
Treatment goals
Management





Remember that prolactin is inhibited by dopamine!
In panhypopituitaryism, the anterior pituitary hormones are more commonly affected than the posterior pituitary hormones and there is a spectrum for how much of the HPA axis is still preserved depending on the etiology of the panhypopituitaryism.
The hormones that need replacement in adults are T4 and cortisol. Testosterone can be replaced if needed in men. Estrogen and progesterone can be replaced in pre-menopausal women who do not want fertility at that time or in post-menopausal women to relieve post-menopausal symptoms. If a woman desires fertility and has enough HPA axis preserved then patients can get pulsatile GnRH to stimulate FSH and LH production to induce ovulation.
To screen for adrenal insufficiency, check a morning cortisol at 8am.
Stimulation tests
Adrenal crisis
Remember – if you suspect adrenal insufficiency, give stress dose steroids immediately without waiting for further testing!





Definition: mPAP greater or equal to 25 mmHg at rest
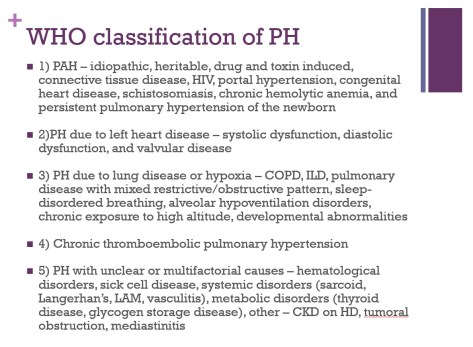
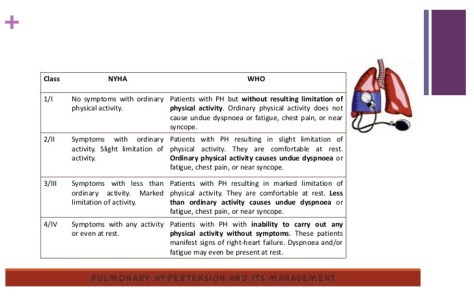
Symptoms
– Most common is dyspnea
– Other symptoms include exertional chest pain due to increased myocardial oxygen demand from enlarged right ventricle and increased pressure, peripheral edema, and anorexia (from hepatic congestion)
Diagnostic evaluation
– Transthoracic echo as screening and if evidence of heart disease then likely group 2
– If no evidence of left heart disease then check PFTs, overnight oximetry, VQ scan, LFTs, HIV, ANA, etc to rule out other etiologies of PH
– Patients only need a RHC for confirmation or if other cause of possible PH does not fit the extent of PH seen
– Vasoreactivity testing – if positive then patient would benefit from CCB
– Positive vasoreactivity test is a drop in mPAP of at least 10 and less than 40 mmHg overall without hypotension or drop in CO
Treatment
– For group 2-5 treat the underlying cause
– If evidence of PaO2 < 60 in group 3 then start oxygen
– Treat with anticoagulation to prevent further clots in CTEPH but only definitive treatment is thrombectomy
– For group 1 – can use vasodilators, anticoagulation (because high risk of PE in these patients), digoxin for right heart contractility, and diuretics for volume management