Credit goes to Dr. Scott Burns from Roper Hospital in Charleston for his case on the Human Diagnosis Project.
Today we discussed a case of a young man with otherwise no medical history presenting with subacute dry cough, malaise, and weight loss. On exam he was septic on presentation with notable oral thrush. CXR revealed bilateral interstitial infiltrates and a RUL cavity with air fluid level which was confirmed on CT. LDH was elevated. He was confirmed HIV positive with a low CD4 count in the single digits, and BAL confirmed the diagnosis of PCP/PJP pneumonia!
Oral Thrush: NEVER assume normal, extremely rare in immunocompetent patients, so if you see this, consider whether the patient could be immunocompromised.
Cavitary Lung Lesion DDX
- Mycobacteria
- Bacterial
- Pseudomonas
- Enterobacteriaceae
- Klebsiella
- Streptococci
- Nocardia
- Anaerobes
- Staph aureus
- Fungi
- Crypto
- Aspergillus
- Histoplasma
- Rare
- Bacterial: Legionella, rhodococcus
- Mycobacteria: MAC
- Fungi: PCP/PJP, mucormycosis, blasto
- Others: Vasculitis
PCP
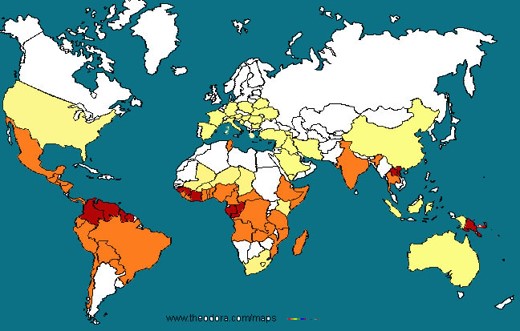
Epidemiology
- Immunocompromised patients
- HIV with CD4 < 200
- BMT, organ transplant patients
- Leukemia/lymphomas
- Rheumatology conditions
- Primary immunodeficiencies
- Rarely occurs in immunocompetent patients
Presentation
- Typically subacute onset of pulmonary symptoms, non-productive cough, fever chills, malaise, SOB
- Might have other clues of immunocompromised status
Diagnosis
- CXR: Classic description is bilateral interstitial infiltrates
- Rare instances: Lobar infiltration, nodules, cavitary lesions, pneumothorax
- CT: Higher sensitivity but might not be necessary for the dx
- LDH: Sensitive but not specific if elevated. An elevated LDH in an HIV patient without other medical co-morbidities that might inc LDH should raise suspicions for PCP
- Beta D glucan: For HIV patients, good sensitivity, not that specific. If elevated, raises suspicions for PCP.
- Gold standard: either visualize the organism via induced sputum (yield is variable, variable sensitivity but 100% specific), or via BAL.
- Can also use 18S PCR
Management
- First line: TMP-SMZ, 15-20 mg/kg. PO just as good as IV, duration 21 days
- Sulfa allergy:
- Mild to moderate: Desensitization
- Severe: alternative agents
- Clinda + primaquine
- Trimethoprim + dapsone
- Atorvaquone
- Pentamidine
- For severe disease, Clinda + primaquine or IV pentamidine is preferred.
- Adjunctive steroids
- ABG: If PaO2 < 70, or Aa gradient > 35, or hypoxemia on pulse ox, adjunctive steroid is indicated and has been shown to improve mortality
- Pred 40mg BID x 5 days, then 40mg daily x 5 days, then 20mg daily x 11 days, total 21 days
Remember your Aa gradient equation!
Aa-gradient = PAO2 (calculated from the alveolar gas equation) – PaO2 (measured PaO2 on ABG)
PAO2 = FiO2 (baromeric pressure – water pressure) – PaCO2/(respiratory quotient)
Assuming sea level and a standard respiratory quotient of 0.8, this equation can be simplified to:
PAO2 = 150 – PaCO2/0.8