Ernest presented an interesting case of a middle aged man with h/o CVA presenting with symptomatic megaloblastic anemia, found to have vitamin B12 deficiency induced thrombotic microangiopathy!
Clinical Pearls:
- A “pseudo” TMA can develop in patients with severe vitamin B12 deficiency via red cell destruction in the bone marrow, leading to high LDH but modest rise in total bilirubin.
- B12 related hemolysis is similar to TTP so the latter must be ruled out!
- Treatment involves aggressive vitamin B12 replacement and is not responsive to plasmapharesis.
Differential for megaloblastic (MCV >120) anemia:
- Vitamin B12 deficiency (elevation of both MMA and homocysteine)
- Folate deficiency (elevation of homocysteine alone)
- Drug induced (methotrexate, hydroxyurea, zidovudine, azathioprine, 5-FU, acyclovir, capecitabine)
- Copper deficiency
When schistocytes are on the smear –> non-immune hemolysis.
Primary TMA syndromes:
- TTP
- Low levels of ADAMTS13
- Renal failure, neurologic changes, fever, schistocytes, thrombocytopenia
- Classic pentad only seen in 1/3 of patients
- Triad of elevated LDH, schistos, and thrombocytopenia? –> check ADAMTS13
- Shiga toxin mediated HUS
- Shigella and certain serotypes of E Coli such as O157:H7 and O104:H4.
- Classically with renal dysfunction and HTN as predominant findings
- Bloody diarrhea
- More common in children
- Complement mediated
- Hereditary deficiency of regulatory proteins in the alternative complement pathway
- Drug mediated
- Quinine, quetiapine, immunosuppressants, chemotherapy, calcineurin inhibitors
- Metabolism mediated
- Cobalamin C deficiency (inborn error of metabolism)
- Mutations in the MMACHC gene (methylmalonic aciduria and homocystinuria type C)
- Coagulation mediated
- Hereditary deficiency of proteins in the coag pathway
Systemic disorder associated with MAHA and thrombocytopenia:
- Pregnancy complications (HELLP)
- Severe HTN
- Systemic infections (bacterial endocarditis, HIV, CMV, RMSF)
- Malignancies (with or without DIC)
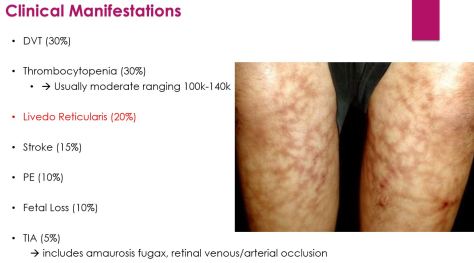
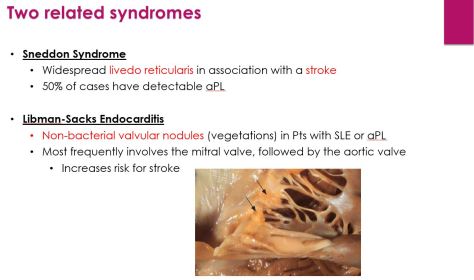
- Autoimmune diseases: SLE, systemic scleroderma, APLS.
- DIC
- Severe vitamin B12 deficiency
Final note on pernicious anemia:
- Most common in Nothern Europeans
- Check in people with vitamin B12 deficiency and no other identifiable cause
- Intrinsic factor antibodies are the test of choice
- Low sensitivity but high specificity
- High sensitivity but low specificity (seen in other autoimmune disease as well as healthy individuals without autoimmune disease)
- What about Schilling test?
References:
Acharya et al. Hemolysis and hyperhomocysteinemia caused by cobalamin deficiency: three case reports and review of the literature. J Hematol Oncol. 2008.