Thanks to Julie for presenting the case of a middle-aged man with recent CAP who presented with progressive SOB, pleuritic chest pain, weight loss, and anorexia, found to be septic with a large empyema, eventually requiring open decortication!
Clinical Pearls
- Think of parapneumonic effusions in two broad categories: infected (complicated and empyema) and sterile (uncomplicated).
- Infected (complicated and empyema) require chest tube placement and can be complicated by loculated effusions.
- Uncomplicated resolve with the treatment of underlying pneumonia
- Anaerobic organisms are a common cause of infected parapneumonic effusions. Malodorous fluid at the time of thoracentesis is diagnostic! But make sure to send anaerobic cultures to the lab to help with speciation.
- pH of pleural fluid can be falsely elevated if not immediately stored on ice upon collection and processed in a blood gas analyzer.
- Differential for pleural fluid that has low glucose/low pH is short: infection, TB, malignancy, rheumatoid pleurisy, and lupus pleuritis.
- Remember that while ADA has high sensitivity (86%) and high specificity (87%) for TB, the study on which it is based was done in a high risk population so its utility in screening low risk patients is limited.
Parapneumonic effusions:
- Form in 40% of bacterial pneumonia:
-
- Uncomplicated: negative GS and Cx, pH>7.2, glucose >60, no loculations
- Complicated: positive GS or Cx or pH <7.2, or glucose <60. LDH >1000 makes it more likely
- Empyema: frank pus aspirated during thora, cell count with >50k WBCs
-
The latter two categories require chest tube placement to prevent formation of pleural “peels” that can lead to trapped lung and loss of lung function.
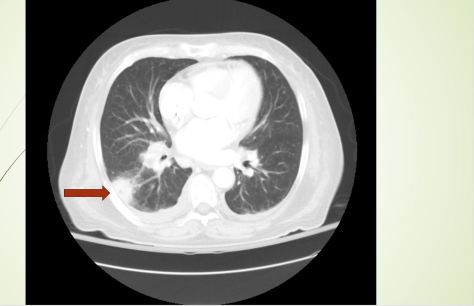
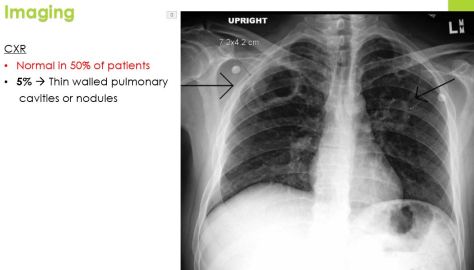
- Imaging
- Lateral decub or ultrasound, latter is more sensitive than CXR for diagnosing complicated parapneumonic effusions.
- CT with contrast is the optimal imaging for empyema or loculated effusion
- Look for the “split pleura sign”
- Labs:
- Serum procalcitonin >0.18 ng/mL is 83% sensitive and 81% specific for effusion having a bacterial infectious etiology
- Bacteriology:
- Anaerobic bugs are often the culprit! So it is important to send pleural fluid for both aerobic and anaerobic cultures
- Other bacteria: CAP organisms such as strep and staph as well as klebsiella in diabetic patients
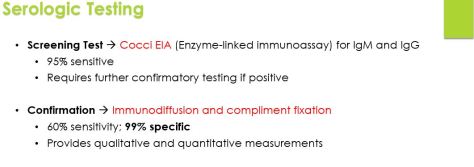
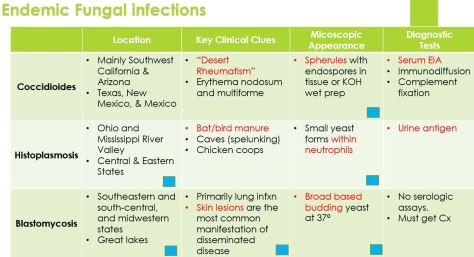
- Fungi
- TB
- Treatment:
- Tube thoracostomy (chest tube): first intervention
- CT within 24 hours to ensure correct positioning and adequate drainage, left in place until drainage is <50 cc/day
- Fibrinolytic agents
- DNA is a main contributor to viscosity of empyema fluid. However, based on this trial published in NEJM in 2011, tPA and DNAase combined is associated with significant radiographic improvement of empyema, reduction in hospital stay, and lower number of surgical referrals.
- VATS
- Decortication
- To remove the thickened fibrin layer covering the pleura.
- Open thoracostomy
- Rib resection and opening the chest wall at the inferior border of empyema to allow for ongoing drainage. High risk of infection and complications.
- Tube thoracostomy (chest tube): first intervention