We discussed a middle aged man with heavy alcohol use presenting with jaundice found to have profound liver failure. It is important to note acute liver failure warrants consideration for transplant candidacy urgently. However, previous records revealed this patient had a history of cirrhosis and prior alcoholic hepatitis, this patient likely suffered from acute on chronic liver failure from alcoholic hepatitis. We reviewed the broad differential for jaundice and specifically for conjugated hyperbilirubinemia (attached). Alcoholic hepatitis may manifest as fever, jaundice, hepatomegaly and leukocytosis. Maddrey’s DF score is used to prognosticate. A score >32 warrants consideration of corticosteroids. STOPAH trial shows nonsigifnicant survival advantage at day 28 in patients with prednisolone vs no prednisolone.
Category Archives: Morning Report
Seizures due to Neurocysticercosis
- Check the patient’s ABCs and IV access
- Check for hypoglycemia
- Ativan 2-4 mg IV pushes x3
- Status epilepticus:
- continuous seizure that lasts ≥5 min OR
- ≥2 discrete seizures w/out return to neuro baseline between seizures
- Neuroimaging can definitely diagnose neurocysticercosis
- Serologies can be helpful. The test of choice is enzyme-linked immunoelectrotransfer blot (EITB)
- Antiparasitic therapy can cause degeneration of cysticerci -> inflammatory response.
- In patients with ocular disease, the inflammatory response can cause edema and lead to blindness. Therefore, always consult ophthalmology to rule out ocular neurocysticercosis prior to starting antiparasitics.
- In patients with CNS disease, the inflammatory response can cause edema and lead to seizures. Therefore, concomitant corticosteroids with antiparasitic medications (and AEDs) is recommended.
Hypercalcemia and multiple myeloma
- If elveated urinary calcium, think primary hyperparathyroidism
- If normal or low urinary calcium, think FHH
- If PTHrP elevated, think cancer
- If high 25 Vit D and high 1,25 Vit D, think excessive PO intake
- If high 1 25 Vit D, think granulomatous disease
- If normal, think medications, immobilization, hyperthyroidism or adrenal insufficiency
Given the hypercalcemia, protein gap, and pancytopenia, the suspicion for multiple myeloma (MM) was high. Subsequent SPEP with immunofixation and bone marrow biopsy confirmed the diagnosis of IgG kappa Multiple Myeloma. Remember that multiple myeloma is a clonal proliferation of plasma cells and bone marrow biopsy with more than 10% plasma cells confirms diagnosis. The monoclonal protein produced by these plasma cells is an abnormal immunoglobulin (immunoglobulin G [IgG], IgM, or IgA, or, rarely, IgE or IgD) and/or light chain protein (kappa or lambda), either of which causes hyperviscosity and/or end-organ damage.
Hypertriglyceridemia induced acute pancreatitis
- R/o emergencies: obstruction, perforation, vascular, ectopic pregnancy.
Hypertriglyceridemia-induced acute pancreatitis
- Triglycerides are broken down into free fatty acids that accumulate to toxic levels, which can cause inflammation of the pancreas.
- Early (within ~48 hrs) enteral refeeding is encouraged.
- Enteral (PO) feeding is recommended over parenteral (IV) to help maintain intestinal barrier and prevent bacterial translocation from the gut.
-
Insulin is used to treat hypertriglyceridemia-induced acute pancreatitis. Insulin promotes storage of triglycerides and inhibits breakdown of triglycerides into free fatty acids.
Thyrotoxic periodic paralysis
- Thyrotoxic Periodic Paralysis is a channelopathy that causes intracellular shifts of potassium. Low serum potassium does not reflect a total body potassium deficit.
- Common triggers include: high-carb meals (insulin-mediated), stress (adrenergic state), intense exercise.
- Repletion of potassium should be gradual (~90mEq in 24 hrs) to prevent rebound hyperkalemia.
Vasospastic angina
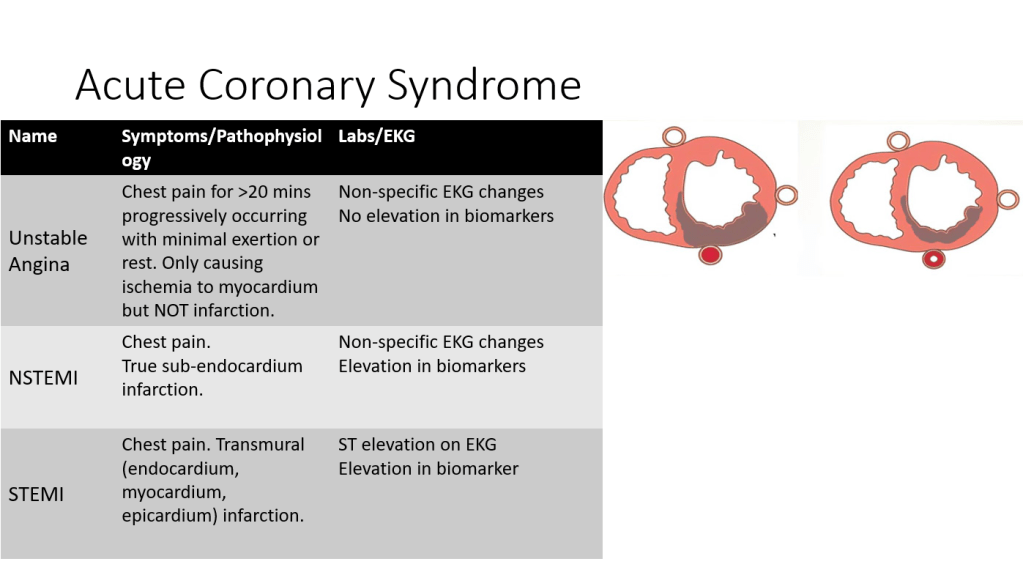
We discussed a case of a middle aged man presenting with acute onset chest pain and bradycardia in the setting of recurrent syncope. Our patient had negative troponins but ST elevations that met criteria for STEMI. STEMI alert was called, however repeat EKG did not meet STEMI criteria. Patient was admitted for unstable angina and received a stress test during which he experienced chest pain with EKG evidence of STEMI. Coronary angiogram was negative for coronary artery disease however he responded to intracardiac nitroglycerin with significant increase in the caliber of left PDA. He was diagnosed with a type of MINOCA (MI in the absence of obstructive CAD), known as vasospastic angina.
It is important to think of “do not miss” chest pain differentials using the 4:2:1 method:
- 4 cardiac for 4 chambers – ACS, Tamponade, Aortic Dissection, Myocarditis
- 2 pulmonary for 2 lungs – Pulmonary emboli, pneumothorax
- 1 GI tract – Esophageal rupture
Our patient had a STEMI alert called however not all ST elevations equal to STEMI. It is important to know criteria for STEMI:
- ST segment elevation of >1mm at J in two contiguous leads other than leads V2-V3
- In leads V2-V3 >2mm in men older than 40yo and >2.5mm in men younger than 40 yo or >1.5mm in females
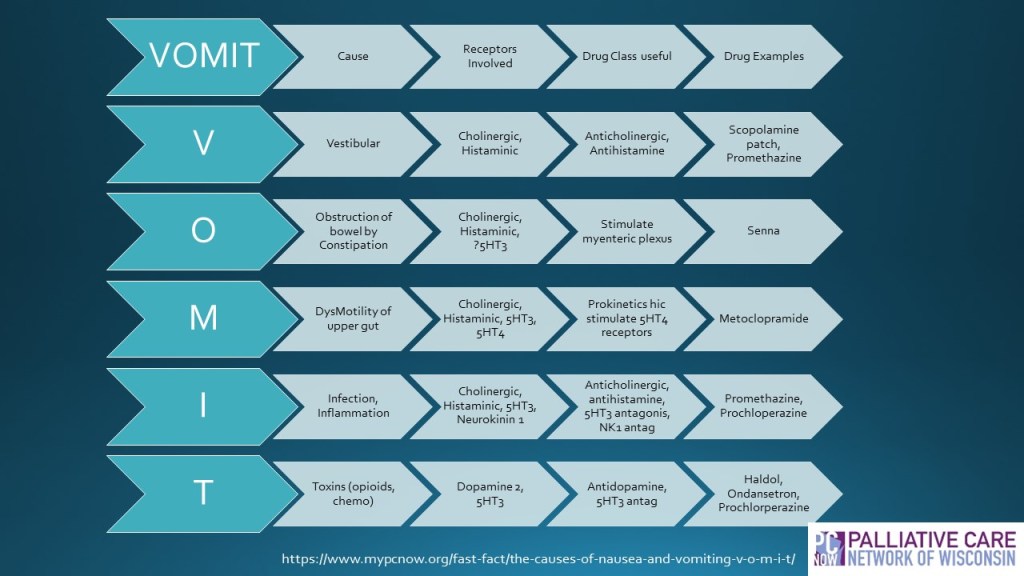
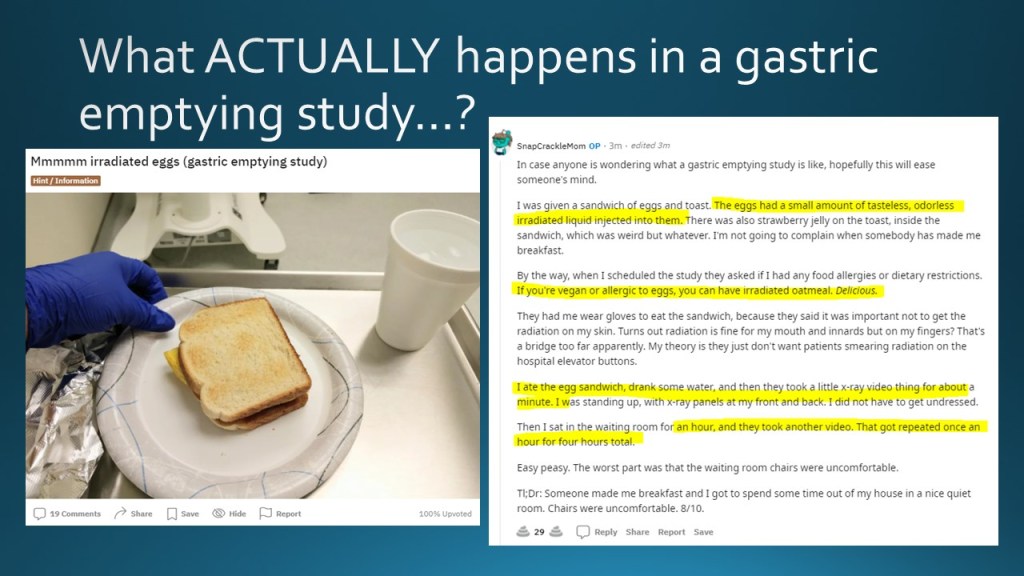
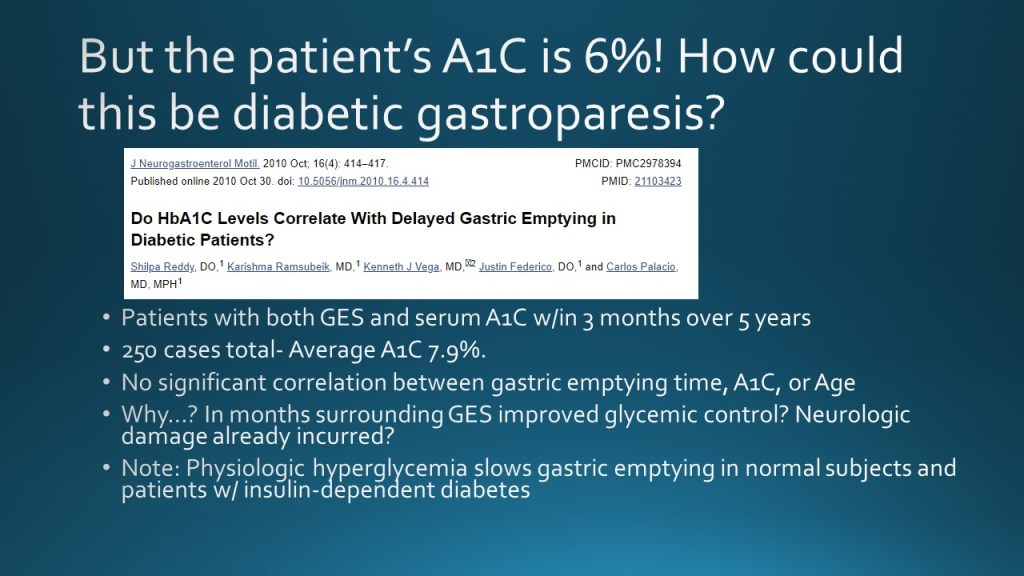
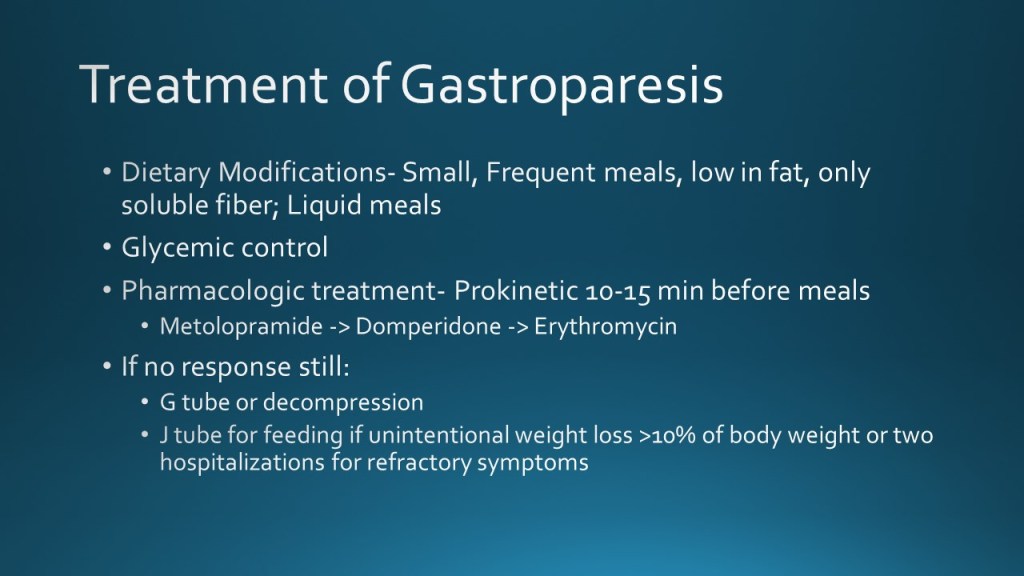
Gastroparesis
Today we discussed the case of an elderly woman with history of diabetes and afib who presented with subacute onset nausea/emesis and epigastric abdominal pain, with gastric emptying study showing marked delayed gastric emptying with >90% of food retained at 4 hours.
We discussed a framework for nausea/emesis as well as how to approach and treat gastroparesis.
Nausea/Emesis can be broken into Acute and Chronic etiologies.
Common etiologies for ACUTE nausea/emesis:
Infections- acute gastroenteritis
Postop Nausea/Emesis- 1/3 of surgical pts have nausea/emesis or both after general anesthesia
Vestibular Neuritis- Rapid onset severe vertigo w/ nausea/emesis, gait instability
Chemo- Common; Anticipatory antiemetic indicated when highly emetogenic chemo regimen given
Common etiologies for CHRONIC nausea/emesis:
Gastroparesis – delayed gastric emptying w/o mechanical obstruction – idiopathic, diabetic
GERD
Gastric Outlet obstruction- pyloric stenosis from malignancy or PUD
Chronic idiopathic
Functional nausea/vomiting disorder
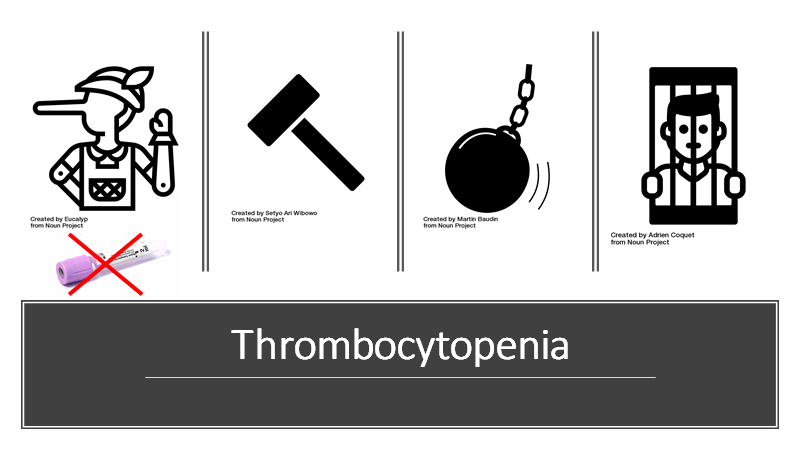
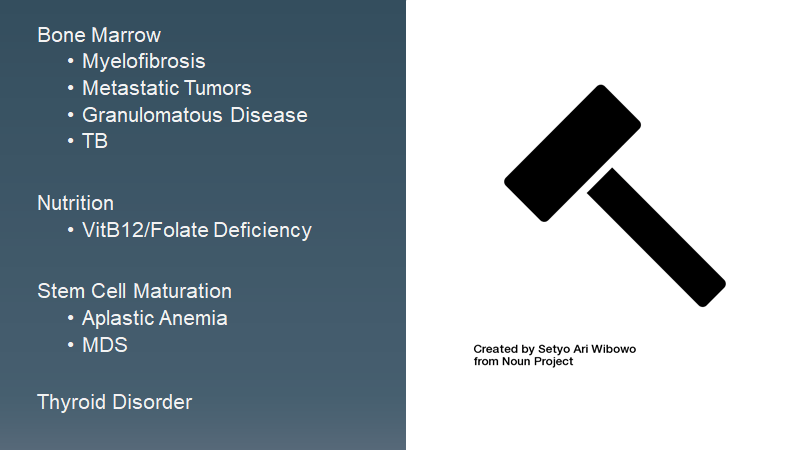
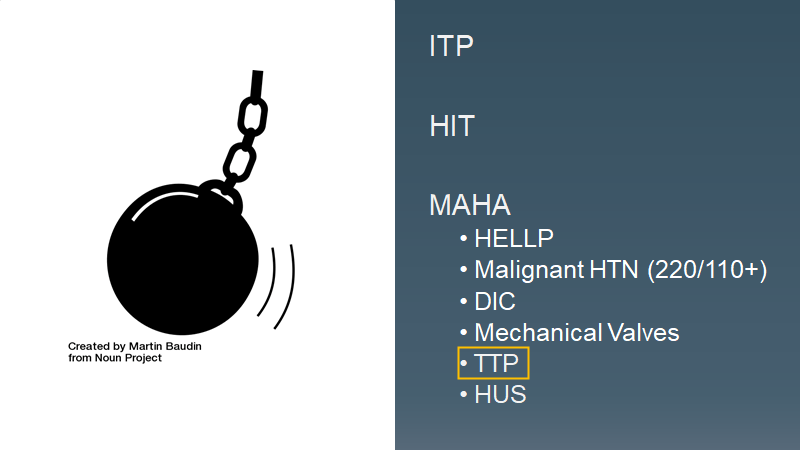
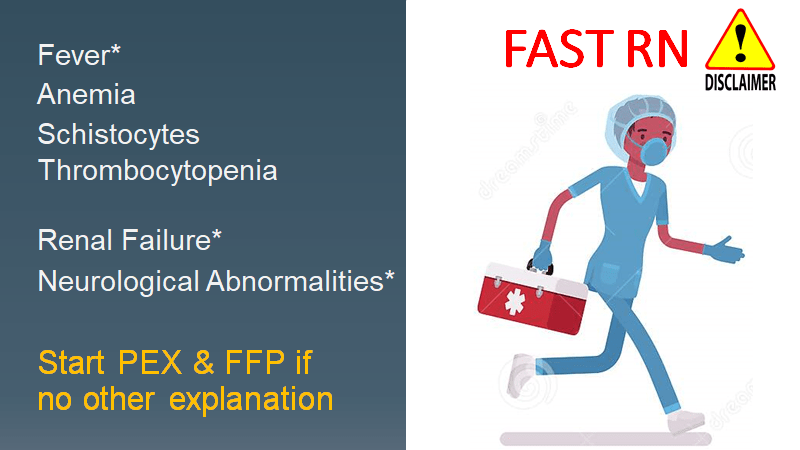
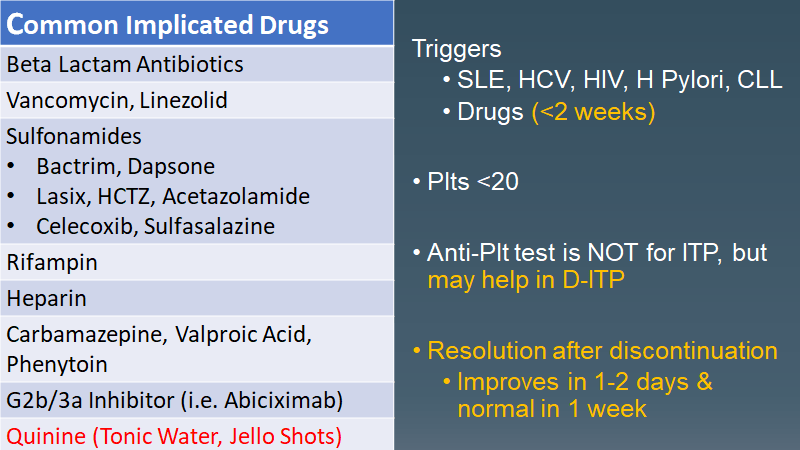
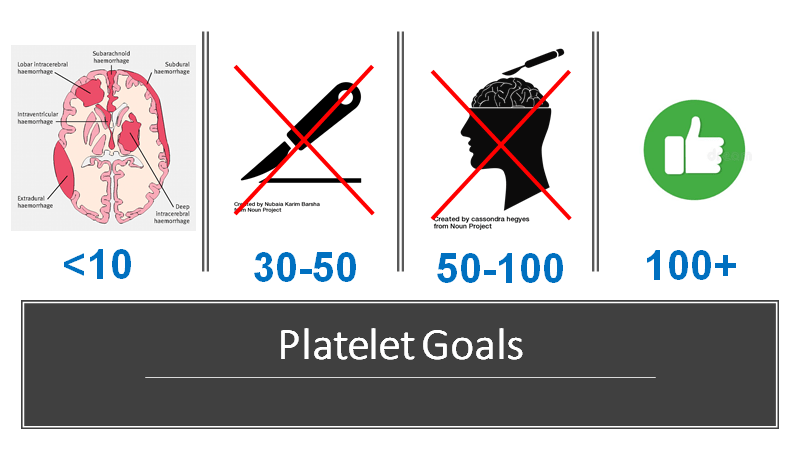
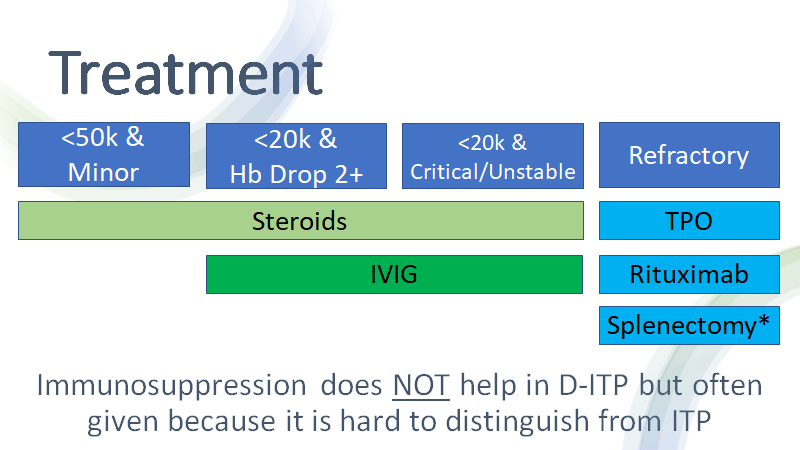
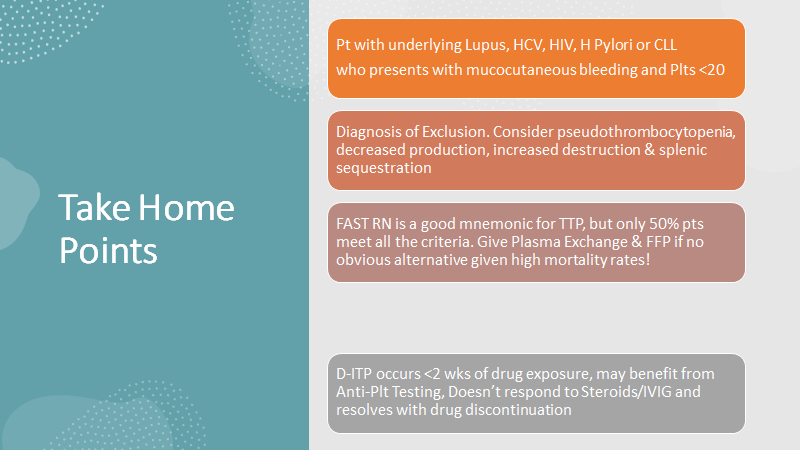
Drug-induced ITP
Peritoneal Tuberculosis
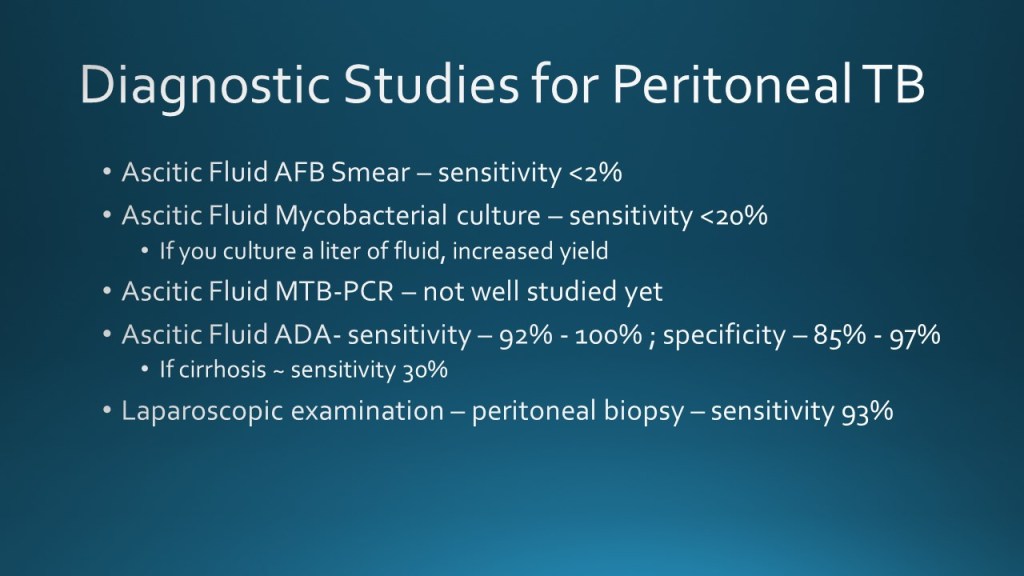
Earlier this week, we discussed the case of a young woman who immigrated from Mexico as a child, who presented with subacute fever, increased abdominal girth and acute onset abdominal pain, nausea, and PO intolerance found to have ascites with SAAG <1.1 consistent with exudative ascites, and diffuse peritonitis on CT.
We reviewed the differential for exudative ascites as the following:
Peritoneal Carcinomatosis
Peritoneal Tuberculosis
Pancreatitis
(additionally serositis, nephrotic syndrome, bowel perforation/infarction)
We reviewed the diagnostic studies for peritoneal TB and notably learned that elevated ascites fluid adenosine deaminase level is particularly helpful in supporting in a diagnosis of peritoneal TB and against diagnosis of peritoneal carcinomatosis.
We reviewed the utility of different imaging modalities when suspecting gynecologic malignancy, notably Ultrasound being first line imaging modality, MRI having the role of detecting pelvic extent of disease and local staging, and finally CT and PET/CT to evaluate extra-pelvic disease and distant metastases.
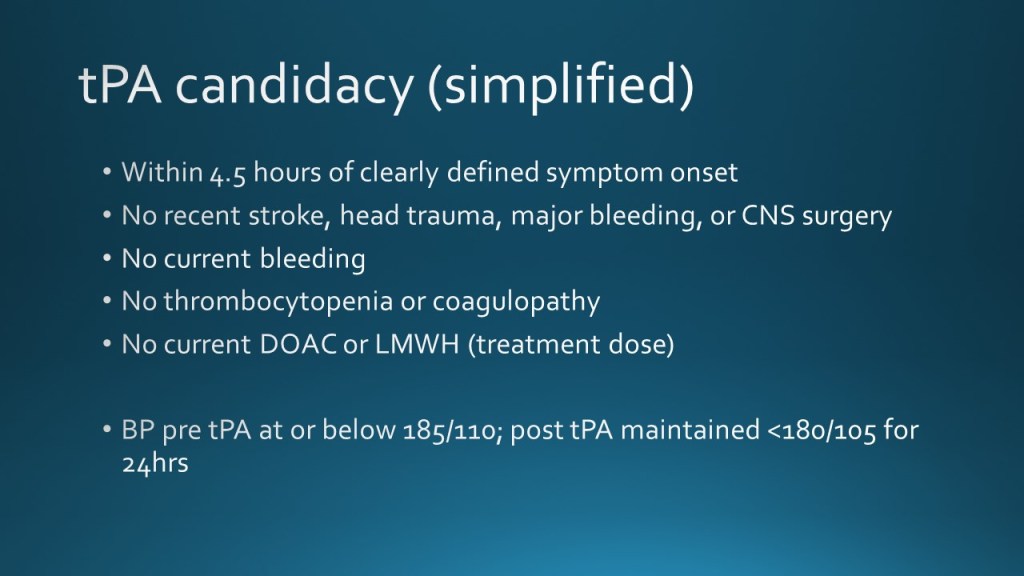
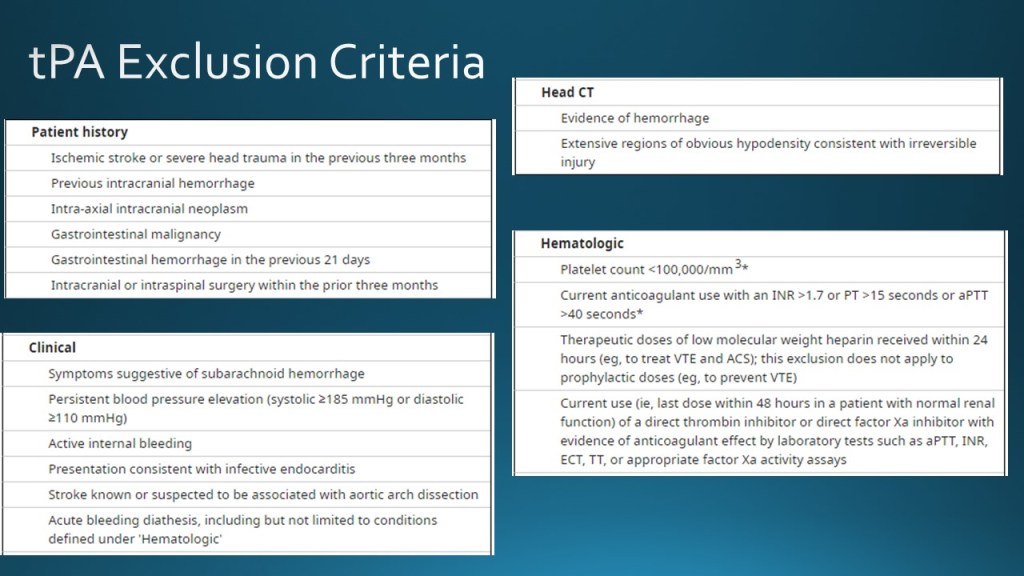
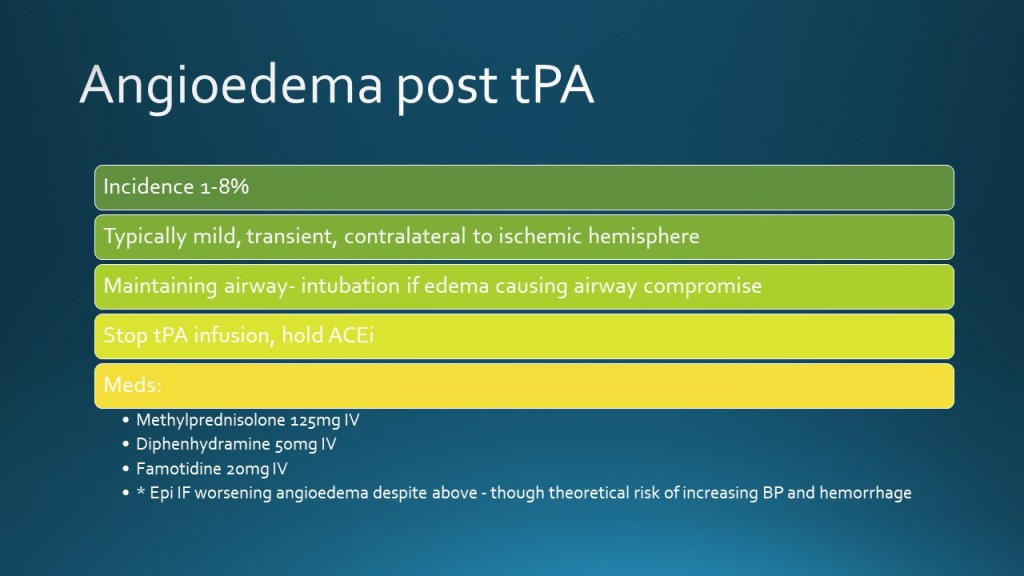
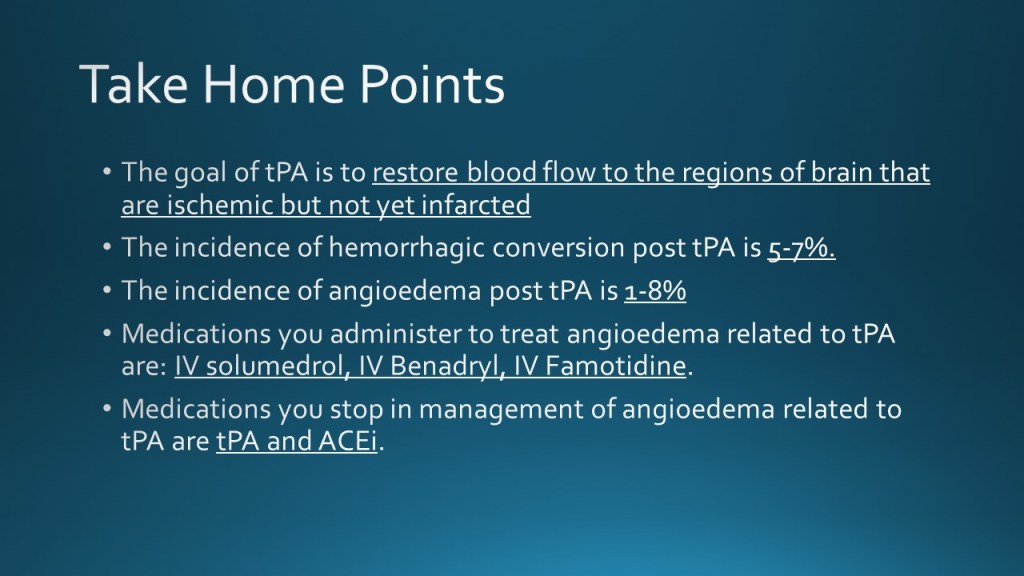
post-tPA complications; hemorrhagic conversion and angioedema
Today we discussed the case of an elderly woman with prior history of ischemic stroke, HTN, HLD who presented with dysarthria and hemiplegia found to have an acute ischemic stroke for which she was given tPA with subsequent hemorrhagic conversion and angioedema.
We reviewed inclusion and exclusion criteria for tPA administration and discussed managed of angioedema post tPA.